06 May Should Pregnant Women Get the COVID-19 Vaccine?
By Emily A. McInnis, D.O.
As some of our patients already know, my husband and I are expecting! It’s an interesting time to be pregnant due to COVID-19 and the vaccines that we currently have available. There are many opinions out there, but it’s also important to be sure that the decisions you are making regarding your pregnancy and your baby are safe, sound, and based on accurate information.
Armed with that knowledge, the short answer to the question of, “Should I get vaccinated if I am pregnant?” is that it’s truly up to you to decide what’s best.
From my unique perspective of not only being pregnant right now, but also being an OB-GYN, I want to offer my experience regarding the COVID-19 vaccine and provide my professional recommendations for our patients who are pregnant, may become pregnant, and those who are breastfeeding.
Getting the COVID-19 Vaccine While Pregnant
I recommend that pregnant patients receive the COVID-19 vaccination if they desire it. I received the Pfizer vaccine when I was 20 weeks pregnant, after I had my anatomy scan at 18 weeks. I purposefully waited until this point in pregnancy because this is after organ formation has occurred. However, there is no science behind that; it’s just my personal preference.
We have several pregnant patients who have had questions about receiving the vaccine during their pregnancy. It is completely understandable to be concerned about something that is fairly new with so many unknowns. I share my thoughts and the research that I have read and feel comfortable with, but ultimately, I tell patients that it is their choice and their right to decide if getting vaccinated is what they want for themselves and their babies.
Several patients have chosen to get vaccinated and several have chosen not to get vaccinated. There is no wrong answer! We want everyone to do what you feel is right for you and feel comfortable with your choice.
Why Pregnant Women Should Consider the COVID-19 Vaccine
As a doctor, my reasons for getting the vaccine may be a little different, but I did have several reasons that I will share. First, with my job I am around COVID+ patients daily, especially in the hospital. I knew that my chances of getting COVID were higher than average, and I did not have the choice to work from home and stay distanced from patients who were positive. My patients need me to take care of them, and that’s what I will do!
While the known absolute risk is low, pregnancy is associated with increased risk of maternal severe illness, ICU admission, mechanical ventilation, and death from COVID-19. There is also a known increased risk of complications from COVID-19 in pregnant patients with underlying health conditions (e.g. diabetes, obesity, increasing age, and cardiovascular disease).
I have personally seen one case and heard of several other cases of pregnant patients who had Covid during their pregnancy that they recovered from, but they had issues postpartum, such as neurological deficiencies or low platelets/DIC/bleeding issues. There is also a risk of preterm delivery or preeclampsia with COVID+ pregnancies. I did not want to take any of those risks that result from actually having COVID-19. I felt that the better choice for me was to get the vaccine.
The most asked question I hear is: “Will this affect or hurt my baby?” The difficult aspect of new vaccines, treatments, medications, etc. is that it is extremely hard to get it through a clinical trial. This is partially due to requirements and the companies making it harder to obtain permission to do trials on pregnant women, but it’s also partially because there are not many pregnant women willing to be the “guinea pig” to try things out when it could potentially affect your unborn child.
However, newer studies are actually showing that not only is the vaccine safe for baby, but newborns are being tested and have antibodies to COVID-19 if the mom has received the vaccination during her pregnancy.
The Science Behind COVID-19 Vaccines
The Pzifer and Moderna vaccines are mRNA vaccines that deliver a message to your body instructing muscle cells in the arm to make a small part of the virus, or a spike protein. The mRNA then degrades quickly while the body develops an immune response to the spike protein. This is not a live vaccine, and in general, these are safe in pregnancy and many are routinely given, such as influenza and Tdap vaccines.
Pregnant women were not included in the initial COVID-19 vaccine clinical trials; however, observational data from vaccinated pregnant individuals is currently being collected by the CDC and manufacturers. One database in particular is called V-Safe Pregnancy Registry through the CDC, which I have registered with myself. Based on limited self-reported information, no specific safety signals have been observed in pregnant women.
Data from Developmental and Reproductive Toxicity (DART) animal-model studies for the Pfizer, Moderna, and Johnson & Johnson vaccines have not demonstrated any safety concerns in pregnancy or future fertility. Based on the mechanism of action of these vaccines and the demonstrated safety and efficacy in Phase II and Phase III clinical trials, it is expected that the safety and efficacy profile of the vaccine for pregnant individuals would be similar to that observed in non-pregnant individuals.
What About the Nursing Mom?
COVID-19 vaccines should be offered to lactating individuals just as they are offered to non-lactating individuals. Based on how these vaccines work in the body, COVID-19 vaccines are not thought to be a risk to those who are lactating or their breastfeeding babies.
Recent reports have shown that breastfeeding women who have received COVID-19 mRNA vaccines have antibodies in their breast milk, which could help protect their babies. More data are needed to determine what protection these antibodies may provide to the baby.
What to Expect When You Get the COVID-19 Vaccine While Pregnant
In my experience, I had very minimal arm soreness for the first 24 hours after both the first and second vaccine shots. I had no other symptoms whatsoever. No headache, nausea, fatigue, weakness, etc. I did take a dose of Tylenol extra strength after both doses.
However, just as with anyone else, pregnant women may experience side effects after vaccination, such as injection site pain and systemic effects, such as fever, muscle pain, joint pain, headaches, fatigue, and other symptoms. Acetaminophen is recommended for pregnant women if desired for prevention or treatment of side effects. Remember that while these side effects may not be present, they are a normal part of the body’s reaction to the vaccine, and they occur as you are developing antibodies to protect against COVID-19 illness.
It is important to note that the American College of Obstetrics and Gynecology (ACOG) has published a statement saying that pregnant patients should be aware of the rare risk of TTS (thrombosis with thrombocytopenia syndrome) after receipt of the Johnson and Johnson COVID-19 vaccine, but that other FDA-authorized COVID-19 vaccines are available, which would include the Pfizer and Moderna mRNA options.
Pregnant Women Can Get the COVID-19 Vaccine If They Choose
Overall, the COVID-19 vaccine is safe during pregnancy, and there is currently no evidence that any vaccines, including COVID-19 vaccines, cause fertility problems. The CDC does not recommend routine pregnancy testing before COVID-19 vaccination. If you are trying to become pregnant, you do not need to avoid pregnancy after receiving a COVID-19 vaccine. Like with all vaccines, scientists are studying this one carefully for side effects now and will report findings as they become available.
If you decide to get the vaccine, here is the vaccine schedule to help you know what to expect:
- Pfizer-BioNtech mRNA: For use in individuals age 16 years and older as a 2-dose regimen given 3 weeks (21 days) apart.
- Moderna mRNA vaccine: For use in individuals age 18 and older as a 2-dose regimen given 1 month (28 days) apart.
- Janssen Biotech Inc. (Johnson & Johnson) monovalent vaccine: For use in individuals age 18 years and older as a single dose regimen.
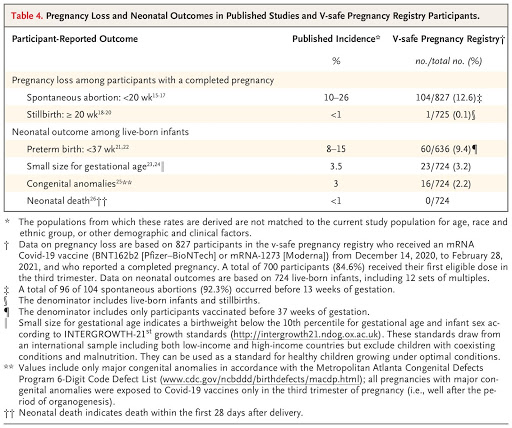
This chart shows that the reported outcomes above were similar (and sometimes even lower) in pregnancies of women who were vaccinated vs. not vaccinated.
We Are Here For You No Matter What You Decide
Regardless of the choice you make, we will support you in your decision, and we hope others will too. I will always be honest about my personal experiences with this, while also providing recommendations based on my professional expertise. While the big question may be whether to vaccinate or not, these conversations provide an opportunity for us to remind patients about the importance of other prevention measures, such as hand washing, physical distancing, and wearing a mask.
LEARN MORE ABOUT WHAT MAKES SYLACAUGA OBSTETRICS & GYNECOLOGY A TOP PROVIDER
Sylacauga OB-GYN is the premier provider of obstetric and gynecological services in Sylacauga, Alexander City, Talladega, and the surrounding areas. From your first exam to your new little one’s delivery, our staff and providers are here to make your journey as smooth as possible. At Sylacauga Obstetrics & Gynecology, we are ready to answer your questions, provide support, and guide your process during your baby’s growth!
No need to drive to Birmingham to receive a superior quality of care for you and your impending bundle of joy. We are big town doctors with small-town care! Give us a call at 256-249-6995 for more information or to schedule an appointment. For more information about healthy pregnancies, delivery options, and more, give us a call or email us at [email protected].